Exhausted from work? Frazzled by your family? Weepy and worried about…well, everything? Choose one—or mix them all together—and you could have the ingredients for depression, a mental health condition that’s blown up like a Deux Moi blind item over the last few years.
Back in 2019, nearly 18 million adults were experiencing depression symptoms. But fast-forward a couple of years and that number explodes: By the end of 2021, with the pandemic in full swing, more than 84 million American adults—almost a third of everybody over the age of 18—were depressed.
Those stats, and the experience of the condition itself, may feel like the end of the world. But they’re not. Depression is highly treatable, and according to the National Mental Health Association, over 80 percent of people who seek help get better. You can, too—here’s what you should know.
What Exactly Is Depression?
Everybody feels down from time to time—that’s just part of being human. But depression is different from that, says Michelle Riba, M.D., a psychiatrist and associate director of the Eisenberg Family Depression Center at the University of Michigan. “It’s a mood disorder, a medical condition with changes that have been taking place for at least a couple of weeks. And it can look a little different for everybody.”
What Are the Signs of Depression in Women?
While only a professional can tell you for sure if you have depression, Dr. Riba suggests first taking an honest assessment of your mood. “Have you noticed any changes in your feelings or behaviors over the past few weeks? If you’re a marathon runner and suddenly you don’t want to get off the couch, think about why you don’t have the energy or desire to do the things you love.”
Keep an eye out for these red flags, especially if they’ve gone on for two weeks or more—or if they’ve been getting worse.
- Changes in your sleep patterns: Tossing and turning? Or sleeping ‘til noon?
- Irritability: Crabby and short-tempered for no particular reason?
- Inability to concentrate: Can’t focus on tasks at home or at work?
- Feeling helpless or hopeless: Seems like things will never get better?
- Relationship issues: More disagreements than usual with your partner?
- Lack of interest in sex: No longer in the mood?
- Aches and pains: Increased headaches or tummy troubles?
If you aren’t sure what emotional place you’re at, you can always try an online self-assessment, like the PHQ-9. “It’s a screening tool, not a diagnosis,” cautions Julia Frew, M.D., a psychiatrist at Dartmouth-Hitchcock Medical Center in Hanover, NH. “But it’s a good starting point.”
Sign up for our free newsletter
Legit tips and cool copes, delivered straight to your inbox.
By completing this form you are signing up to receive our emails and can unsubscribe anytime.
Why Do I Have This? What Causes Depression in Women?
In a People v Depression trial to determine WHO DONE IT, the jury would still be deliberating: As with many mental health conditions, science can’t pinpoint any one cause. But a bunch of factors may play a part.
Brain Chemistry
Neurotransmitters are the chemical messengers that send signals to your brain. You’ve probably heard from your doctor, your friends, and random people on the supermarket checkout line that the feel-good neurotransmitter serotonin is the culprit behind every diagnosis of depression.
The theory goes like this: When you’re low on serotonin, depression is sure to follow. The American Psychiatric Association even includes chemical imbalances in their list of possible causes of depression. But a brand-new report looking at decades of research found no connection between serotonin and depression. So do chemical imbalances lead to depression? In some ways, but it’s more complicated than that, and doctors aren’t 100 percent sure.
Genetics
Like other illnesses, depression can run in the family. “We don’t have a specific gene right now,” says Dr. Riba, “but we do know that depression can be inherited. Long-term studies have shown that even if identical twins are raised apart, if one has depression, the other is likely to have it, too.”
Psychology
You have a greater chance of suffering from depression if you have low self-esteem or are pessimistic or stressed out. In a 2022 study of young adults, researchers found that those who were more optimistic were less likely to be depressed. This is just what it is: We’re not telling you to overnight become a glass-half-full type (as if).
Life Circumstances
If you’ve experienced neglect, abuse, or poverty, you’re more likely to experience depression. And going through something especially difficult recently—say, a breakup or an accident (or a pandemic)—can trigger depression, too.
Sex and Hormones
Studies show a strong connection between reproductive hormones and depression. And one particular hormone, estradiol, may be a big culprit. It’s a form of estrogen that’s involved in ovulation and in thickening your uterus to allow a fertilized egg to be implanted. Young women typically have high levels of estradiol that decrease with age, but a recent study showed that women under age 45 who were depressed had higher-than-normal levels of estradiol. Unusual hormone fluctuations, it turns out, can bring on negative emotions.
Hormones play a big part in why women are at a spiked risk for depression. In fact, women of reproductive age are twice as likely as men in the same group to present with symptoms of depression. “If you’re not pregnant, your body continues to prepare for pregnancy every month, so the hormones are raging,” says Donna Sheperis, Ph.D., a therapist and professor of psychology at Palo Alto University in California.
Health Issues
Sometimes, underlying health problems have a supporting role in depression formation. “Depression may result from health concerns like diabetes, heart disease, and cancer,” says Dr. Riba. “And medications can impact mood and bring on depressive symptoms, too.”
Plus, if you have depression, you’ve also got a 40 percent greater likelihood of developing heart disease. Even younger women are at risk. One study showed that 48 percent of young women who’d had a heart attack reported a previous episode of depression, compared to just 24 percent of men. And when recent heart attack patients were given the PHQ-9 test, young women were more likely than young men to have high scores for depression.
The takeaway: No matter what your age, depression is not all in your head. It can have a big impact on your physical health.
Race and Identity
People who belong to a minority group, studies show, are more likely to experience chronic depression that gets in the way of day-to-day life. “It’s not that depression presents differently among different groups,” explains Dr. Frew, “but more that you’re at a higher risk because of the micro-aggressions and discriminations you face all the time. You’re living in a world where you’re not always treated well.”
In the weeks following George Floyd’s death in 2020, for example, depression and anxiety soared among the Black population, jumping from an already high 36 percent up to 41 percent. And in a 2022 survey, an astounding 58 percent of LGBTQIA+ young people reported depression symptoms, during a time when their very existence is being called into question with damaging legislation in states like Florida and Texas.
“In a country that doesn’t value sexual minorities, depression is much higher among LGBTQ+ people,” says Sheperis. “And for young adults, this stage of life is all about identity development.” In this group, you often face a hostile environment at school and at work—and in many states, new laws curtail (or even eliminate) many of your rights. Nearly 41 percent of LGBTQ+ adults face harassment, including being fired because of their sexual orientation. For LGBTQ+ young people, the increased stress can lead to even greater psychological challenges. “The hostility that comes from the outside can generate anxiety and depression within,” Sherperis says.
How Depression Feels for Women
“There were days when I felt like I was on autopilot. I wasn’t enjoying anything but I was getting it done because I had to. And some days, I was just curled up in a ball on the couch.” —Falla McCallum, 33, a registered nurse in Mississippi
“Decision-making became a huge issue. I couldn’t make up my mind about big and small things, from choosing an ice cream flavor to deciding whether or not I wanted to be a mom.” —Nora*, 35, a graduate student in New Hampshire
*She asked us not to use her real name.
“I was exhausted and stressed out and I told myself to keep trying harder. I felt kind of ashamed of myself that I was in that state. I’d wonder, ‘Why can’t I think myself out of this?’” —Chloe Urban, 42, a nurse in New Hampshire
How Depression Affects Work, Love, and Friends
Think your depression is a deep, dark secret? It’s not. “Sometimes, your family, friends, and coworkers notice your depression before you do,” says Sheperis. “They’re good barometers of when you’re not doing well. They might notice that you’ve been making grumpy, offhand comments that are damaging to your self-esteem, or that you’ve been more down-in-the-dumps than usual.” If your loved ones have been sharing concerns about your well-being, take their comments seriously. After all, they’ve got your best interests at heart.
Plus, they can be part of the treatment. Friendship is a powerful mood-booster—and a big predictor of emotional health. Long-term studies show that loneliness not only increases your risk of depression, it also worsens symptoms if you’re already depressed. That makes nurturing friendships—and listening to your besties—super important.
Now… Let’s move out of the friend zone. For many women, romantic problems and depression are as tied as almond butter and jelly. “They may be feeling irritable and having trouble feeling connected to their partner, and they’re often less interested in sex,” says Dr. Frew. “And some antidepressant meds can impact sexual desire.”
For Falla, the Mississippi nurse, things began to look up when she got out of her bad relationship. But still, her depression lingered. It was only when she went to her primary care provider, who put her on an antidepressant and referred her to a psychiatrist, that she started to crawl out from under the cloud. “He saved my life,” Falla insists. He prescribed an antidepressant and provided talk therapy. That was a big help—and so were the two Yorkie pups she adopted. While there were setbacks, especially when the pandemic hit and nursing school got super-challenging, she made her way through it and came out on the other side.
You certainly don’t need a plus-one to feel fulfilled in life. But data does find a link between singlehood and depression. One long-term study found that at age 22, young women who were single had more symptoms of depression than those who were dating or living with their significant others. And by age 32, women who hadn’t walked down the aisle were more likely to be depressed than their married friends.
But the toughest relationship to navigate with depression? That may be the one you have with yourself. For an “emerging adult,” that can be kind of tricky to navigate. After all, you’re making the transition from school to job, from being single to living with someone who’s more than a roommate, maybe even from being carefree to caring for a small human. And it’s all happening at a time when your brain is still developing.
“In your twenties and thirties, you may be experiencing financial insecurity, relationship insecurity, and you probably haven’t found your career path or discovered what you’re good at or where you’re happy,” says Sheperis. “Young women in their reproductive years bear so much of the burden on their backs—they’re in the fight, in the trenches.”
When New Hampshire nurse Chloe struggled with postpartum depression, getting better seemed all the more difficult because she felt like it was her fault. “I’m an overachiever and a perfectionist, and I kept wondering why I couldn’t handle this,” she recalls. “I was very critical of myself; I was never in a mind frame to step outside myself and look at what was really happening.” She blamed herself.
But depression is never your fault, insists Sheperis. “Cut yourself a break,” she says. “You can’t always pull yourself up by your bootstraps, like they told our grandparents to do. Just sucking it up didn’t work for them, but they didn’t have anything else to turn to. Today there are a lot of good treatments and coping strategies for depression, but avoidance and denial definitely don’t work. You can avoid thinking about it or go out with friends or watch a movie to escape, but that won’t get to the root of your depression.” Don’t be afraid to ask for help.
Let’s Talk About the Best Treatments for Depression for Women
When your doctor diagnoses depression, they’ll get you started on a treatment plan. Most of the time you’ll be given the option of medication or therapy—or a combination of the two. But whatever treatment your doctor prescribes, stay on plan. These are some options that can make you feel better.
Medication
- Selective Serotonin Reuptake Inhibitors (SSRIs). There are a number of antidepressants that get prescribed for depression, but SSRIs are usually the first line of treatment. “They tend to be well tolerated,” says Dr. Frew. “You might get an upset stomach but that goes away in a few weeks. And they won’t make you feel sleepy or sedated—nobody wants to feel like a zombie.But they can take a few weeks to kick in, so don’t get discouraged.” If side effects start to bug you, don’t be afraid to pester your doctor about it. They’ll work with you to find an alternative.
The most common SSRI prescriptions are:
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
- As for how they work, a month ago it would have gone something like this: “by helping the neurotransmitter serotonin pass along ‘feel-good’ messages from one nerve cell to the next, which has a good influence on your mood, your emotions, and even your sleep.” But that new meta-analysis, the one we mentioned above, called that into question, and psychiatrists admit it’s unclear how exactly these meds work but that, for many, they do work, so if you’re currently talking them, you should not stop unless consulting with your doctor.
- Ketamine. Psychedelic party drug? Not anymore. Ketamine has left its bad reputation behind as doctors have begun using it as a superfast treatment for people with severe depression—or for those who haven’t responded to other drugs. Unlike standard medications, which can take weeks to kick in, ketamine can lift depression almost immediately and last for a long time by increasing your levels of the neurotransmitter glutamate.It can be administered by IV injection or—in a newer version called esketamine—as a nasal spray, though doctors often prefer to the IV version. Both are given at the doctor’s office, where you’re carefully monitored for a couple of hours. Studies show that it’s effective for about half of those who receive it, but doctors still don’t know much about long-term effects.
Talk Therapy
Your doctor may refer you to a trained counselor—such as a psychologist, psychiatrist, or clinical social worker—to discuss your concerns and find solutions. Cognitive Behavioral Therapy (CBT) is one of the most effective strategies—that’s when you work with your therapist to identify behaviors and negative thought patterns and come up with ways to replace them. “For me, therapy made a night-and-day difference in my life,” says graduate student Nora. “Little by little, things just became easier and less exhausting. Now, when I look back, I see how far I’ve come.”
Tough to get away from work for a couple of hours? Sneak out to your car with your smartphone and do a 45-minute video session over your lunch break. A 2022 study compared people who got therapy at a counselor’s office with those who got it via FaceTime. The results? Both groups reported less depression and a better quality of life. Plus, telehealth visits are usually cheaper than going to the office—and sometimes even free with insurance.
Electroconvulsive Therapy (ECT)
ECT uses brief electrical impulses to stimulate the brain, administered by a team of doctors, nurses, and an anesthesiologist. Used for people whose depression hasn’t responded to other kinds of therapy, it’s given in five or six sessions over the course of a few weeks.
If it works for you, you’ll need to go back every three months or so for follow-up sessions. It won’t eradicate all your symptoms, but studies show that it helps about 80 percent of people with treatment-resistant depression.
Transcranial Magnetic Stimulation (TMS)
Sounds like science fiction, but it really works. It’s a legit treatment that uses a device that’s approved by the FDA. Using magnetic fields to stimulate areas of the brain, TMS is another effective treatment for people who haven’t responded well to other treatments. It’s performed by a doctor without anesthesia, says Dr. Frew—it’s not painful, but you may experience some pinprick sensations.
The downside: You’ll need about 20 to 40 hour-long treatments over the course of six weeks, and you’ll need to keep going back for more treatments to stay well. Like ECT, it’s not a cure.
3 Things You Should Never Say to Someone Who Shows Signs of Depression
Want to help? Think before you open your mouth. Cheerful pep talks and platitudes can make a friend with depression feel even worse. Here’s what not to say—and a better alternative for each.
1. “You look depressed—cheer up!”
If all it took to cheer up was hearing those two words, depression stats would be a hellavu lot lower. This has the same effect as “calm down” does for someone with anxiety: Not only is it infuriating, it suggests you can just flip a switch and feel better.
Instead, say… “You haven’t seemed like yourself lately. Do you want to talk? I’m here to listen.”
2. “Snap out of it.”
Riiiiight. I’ll do that, ‘k? This lacks empathy and places blame on your friend.
Instead, say… “I know that you are feeling low. What can I do to help?”
3. “It’s all in your head.”
Well, indeed, it is in your head…but not in the way this statement implies. The world’s top doctors don’t even understand all of the complexities that lead a mind to become depressed, much less the person who blurted out this cliché.
Instead, say… “You are important to me and I am here for you.”
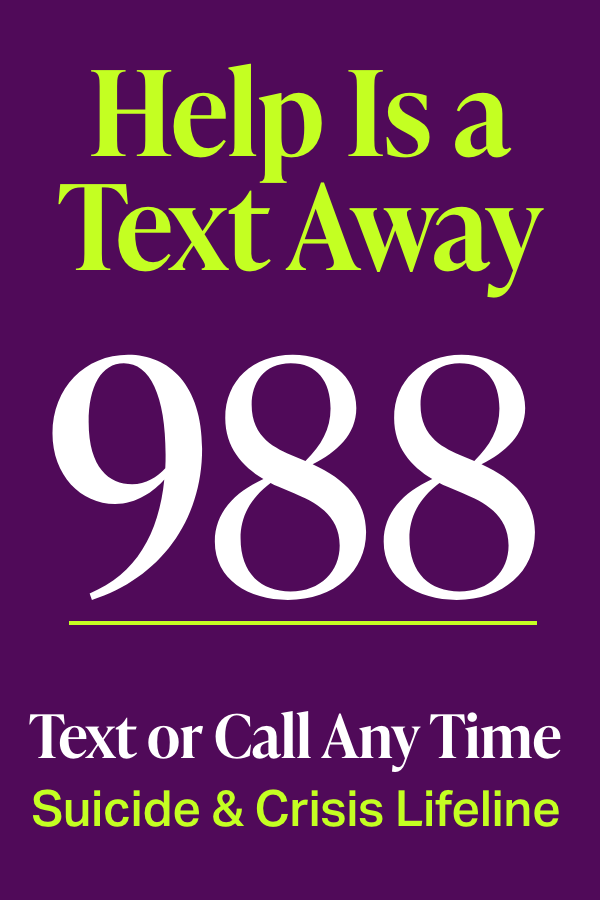
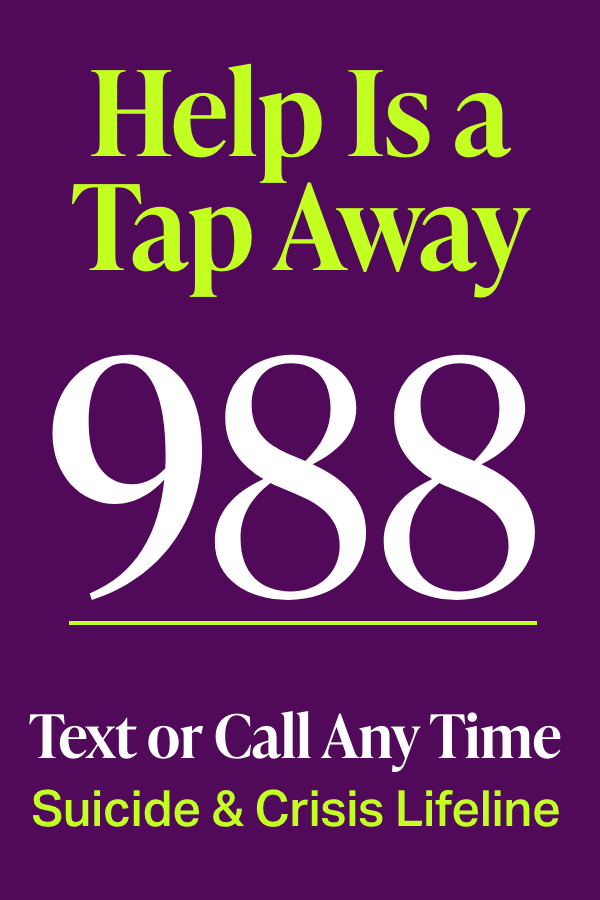
Where to Find Help If You Have Symptoms of Depression
The best place to start, says Dr. Frew, is with your primary care provider, where a full check-up is always a good idea. That’s because other health conditions—or even other medications—can bring on depression symptoms. An underactive thyroid, for example, can launch symptoms that mimic depression, like fatigue and sadness. “So your PCP will ask questions about your general health,” she explains.
If—like lots of other young people—you don’t have a doctor (or health insurance), look for other options. For students, most colleges have a health center with staff experienced in mental health concerns. An urgent care center can be a good place to get an initial assessment, or there may be a free or low-cost health clinic in your community.
But the doctor’s office isn’t your only safe space. You can also find help online through support groups, apps, and others on social media.
The Orgs
National Alliance on Mental Illness. In a special section for young adults, you’ll get ways to choose the right mental health provider, navigate insurance questions, and learn how to share your mental health concerns with your school or employer. Plus, find an online or in-person support group near you.
Anxiety and Depression Association of America. Information, resources, and help locating a therapist.
Centers for Disease Control and Prevention. Take a quiz that helps you figure out if you might be depressed.
Center for Young Women’s Health. A resource that empowers young women, as well as transgender, nonbinary, and intersex young people, to take an active role in their own health care—including recognizing and responding to depression.
Go Ask Alice! Geared toward young adults, this Q-and-A website from Columbia University contains a database of questions about all kinds of emotional health concerns.
Depression and Bipolar Support Alliance. The Young Adult Council features online support groups and podcasts for those between 18 and 29.
The Follows
Julie Smith, @drjuliesmith
Follow because: A TikTok’ing British clinical psychologist on a mission to make top-quality mental health education accessible online. Great advice in fun, quick bites, plus weekly livestreams that let you bring your own questions to the table.
Allyson Dinneen, @notesfromyourtherapist
Follow because: Dinneen, a marriage and family therapist who lives in the Berkshires, offers her IG followers simple ways to rewire their brains to find moments of joy. Scribbled on a piece of scrap paper, torn from a notebook, or scrawled across an old T-shirt, the messages might just be the words you needed to get yourself through a tough spot.
Jessica Clemons, M.D., @askDrJess
Follow because: Find personal anecdotes, daily affirmations, and a weekly livestream where you can ask this psychiatrist questions in real time about everything from handling anxiety and depression to growing in empathy and compassion.
The Apps
There are now a zillion apps purporting to help your mental health. Do they really work? A recent analysis of 18 studies of more than 20 mobile apps showed that they can be effective in relieving depression and helping people manage their symptoms. (They seem to work best for moderate, rather than severe, depression.)
CBT Companion teaches cognitive behavioral therapy techniques through activities, videos, and interactive tools. There’s a journal to log your mood, sleep, and meds. It’s free to get started but a monthly subscription fee unlocks additional features.
Virtual Hope Box has pre-populated content with good mental-health strategies, but you can customize it with photos and videos of loved ones, as well as relaxation exercises and games you enjoy. It was developed by the VA Portland Health Care System and the Department of Defense’s Telehealth and Technology Center to help veterans, and proven to do so in research. Free.
Thought Diary helps you track your moods, identify negative thinking patterns, and reframe your thoughts. Free.
News and Statistics (1): United States Demographic Statistics. Infoplease. May 16, 2021.
News and Statistics (2): 2019 U.S. Population Estimates Continue to Show the Nation’s Growth Is Slowing. United States Census Bureau. December 30, 2019.
Depression Stats (3): Mental Health by the Numbers. National Alliance on Mental Health. April 2023.
Depression Basics: What Is Depression? American Psychiatric Association. October 2020.
Depression Risks: Marsh W, Bromberger J, Crawford S, et al. Lifelong Estradiol Exposure and Risk of Depressive Symptoms During the Transition to Menopause and Postmenopause. Menopause. December 2017.
Serotonin and Depression: Moncrieff J, Cooper R, Stockmann T, et al. The Serotonin Theory of Depression: A Systematic Umbrella Review of the Evidence. Molecular Psychiatry. July 20, 2022.
Pessimism and Depression: Karhu J, Hintsanen M, Ek E, et al. Dispositional Optimism and Pessimism in Association with Cognitive Abilities in Early and Middle Adulthood. Personality and Individual Differences. October 2022.
Depression and the Pandemic (1): Covid: Depression Rises in Young and Women During Second Peak. BBC. May 5, 2021.
Depression and the Pandemic (2): Ettman C, Cohen G, Abdalla S, et al. Persistent Depression Symptoms During Covid-19: A National, Population-Representative Longitudinal Study of US Adults. The Lancet Regional Health Americas. October 4, 2021.
Hormones and Depression (1): Lei R, Sun Y, Liao J, et al. Sex Hormone Levels in Females of Different Ages Suffering from Depression. BMC Women’s Health. May 22, 2021.
Hormones and Depression (2): Reproductive Hormones. Endocrine Society. October 24, 2022.
Gender and Depression: Shi P, Yang A, Zhao Q, et al. A Hypothesis of Gender Differences in Self-Reporting Symptom of Depression: Implications to Solve Under-Diagnosis and Under-Treatment of Depression in Males. Frontiers in Psychiatry. October 25, 2021.
Young Women, Heart Disease, and Depression: Is Depression a CV Risk Factor in Young Women? American College of Cardiology. April 27, 2016.
Race and Depression: Bailey R, Mokonogho J, Kumar A. Racial and Ethnic Differences in Depression: Current Perspectives. Neuropsychiatric Disease and Treatment. February 22, 2019.
Depression in Black Population After George Floyd’s Death (1): Eichstaedt J, Sherman G, Giorgi S, et al., The Emotional and Mental Health Impact of the Murder of George Floyd on the US Population. Proceedings of the National Academy of Sciences. September 28, 2021.
Depression in Black Population After George Floyd’s Death (2): Fowers A, Wan W. Depression and Anxiety Spiked Among Black Americans After George Floyd’s Death. The Washington Post. June 12, 2020.
LGBTQ Mental Health: 2022 National Survey on LGBTQ Youth Mental Health. The Trevor Project. 2022.
LGBTQIA+ Community and Depression: 2021 National Survey on LGBTQ Youth Mental Health. The Trevor Project. 2021.
LGBTQIA+ Community and Discrimination: Lesbian, Gay, Bisexual, Transgender & Queer {LGBTQ}. Gender Equality Law Center.
Loneliness and Depression: Achterbergh L, Pitman A, Birken M, et al. The Experience of Loneliness Among Young People with Depression: A Qualitative Meta-Synthesis of the Literature. BMC Psychiatry. August 24, 2020.
Singlehood and Depression: Grundström J, Konttinen H, Berg N, Kiviruusu O. Associations Between Relationship Status and Mental Well-Being in Different Life Phases from Young to Middle Adulthood. SSM Population Health. March 17, 2021.
Antidepressant Basics: Depression: How Effective Are Antidepressants? InformedHealth.org. June 18, 2020.
SSRI Basics: Overview — Selective Serotonin Reuptake Inhibitors (SSRIs). NHS. December 8, 2021.
Ketamine for Depression Treatment (1): Meisner R. Ketamine for Major Depression: New Tool, New Questions. Harvard Health. May 22, 2019.
Ketamine for Depression Treatment (2): Wray N, Schappi J, Singh H, et al. NMDAR-Independent, cAMP-Dependent Antidepressant Actions of Ketamine. Molecular Psychiatry. December 2018.
Ketamine for Depression Treatment (3): Chen J. Treating Depression: An Expert Discusses Risks, Benefits of Ketamine. Yale Medicine. October 16, 2017.
Cognitive Behavioral Therapy Basics: Psychotherapy. National Alliance on Mental Health.
In-Office Therapy vs Facetime: Cuijpers P, Noma H, Karyotaki E, et al. Effectiveness and Acceptability of Cognitive Behavior Therapy Delivery Formats in Adults with Depression: A Network Meta-Analysis. JAMA Psychiatry. April 17, 2019.
Telehealth vs In-Person Treatment (1): Bulkes N, Davis K, Kay B, Riemann B. Comparing Efficacy of Telehealth to In-Person Mental Health Care in Intensive-Treatment-Seeking Adults. Journal of Psychiatric Research. January 2022.
Telehealth Costs: Bowman C. How Much Does a Telehealth Visit Cost? GoBankingRates. May 25, 2022.
Electroconvulsive Therapy Basics: McDonald W, Fochtmann L. What Is Electroconvulsive Therapy (ECT)? American Psychiatric Association. January 2023
Mental Health Apps and Depression: Chandrashekar P. Do Mental Health Mobile Apps Work: Evidence and Recommendations for Designing High-Efficacy Mental Health Mobile Apps. mHealth. March 2018.
Efficacy of Virtual Hope Box: Bush N, Smolenski D, Denneson L, et al. A Virtual Hope Box: Randomized Controlled Trial of a Smartphone App for Emotional Regulation and Coping with Distress. Psychiatric Services. April 1, 2017.
ADDITIONAL SOURCES
Pescosolido BA, Halpern-Manners A, Luo L, Perry B. Trends in Public Stigma of Mental Illness in the US, 1996-2018. JAMA Network. December 21, 2021.
Cuijpers P, Stringaris A, Wolpert M. Treatment Outcomes for Depression: Challenges and Opportunities. The Lancet Psychiatry. February 17, 2020.
Depression (Major Depressive Disorder): Symptoms & Causes. Mayo Clinic. October 14, 2020.
What Is Depression? American Psychiatric Association. October 2020.
Munsey C. Emerging Adults: The In-Between Age. American Psychological Association. June 2006.