In the mental health world, a debate persists: to pill or not to pill? For some, prescription meds can be lifesaving; for others, they’re not a preferred treatment method. In “The Pill Diaries,” we’ll be telling your stories in your own words. The goal: End pill shaming, bust stigmas, and promote understanding. After all, each person’s journey to better mental health is uniquely their own.
I firmly believe antidepressants saved my life. When I was 14 during my freshman year of high school, I struggled with depression and serious suicidal ideation. It got to the point where if I wasn’t in school or at an extracurricular activity, I was sleeping. I couldn’t motivate myself to study or complete assignments. I felt hopeless and couldn’t imagine a future beyond a few months because I was convinced I wouldn’t still be alive.
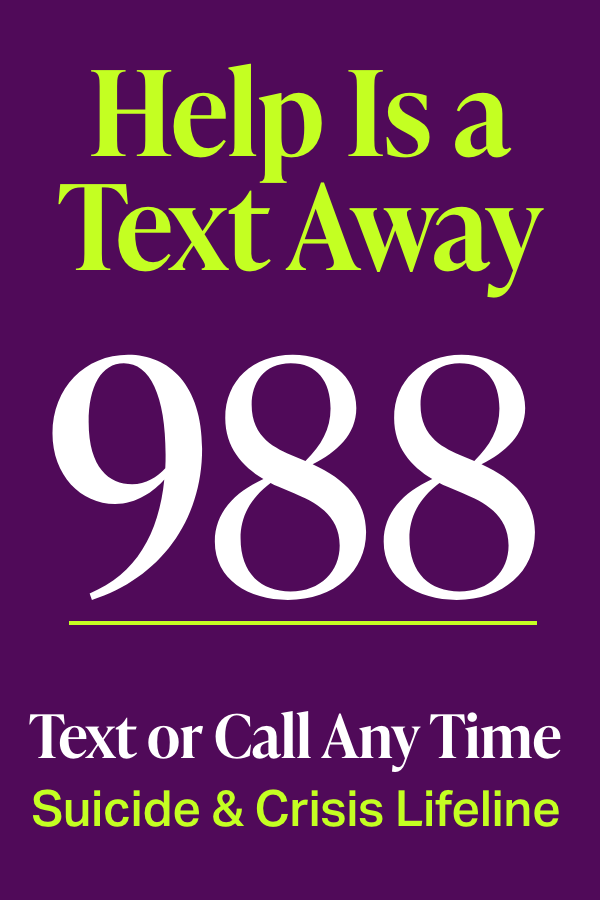
Mental Note: If you are having suicidal thoughts or experiencing a mental health crisis, text or call 988, the Suicide & Crisis Lifeline, any time day or night to speak with a trained counselor.
I was fortunate to have parents who listened to me and took me to get professional help as soon as I opened up about my struggles. After visiting with an adolescent psychologist and pediatrician at a nearby children’s hospital, I was prescribed Zoloft to manage my depression and anxiety. I started on a low dose, which helped for a little bit, but I still had suicidal thoughts and depressive episodes. With each visit to my doctor, we titrated up the dose until I was taking 150 milligrams a day (the standard highest dose for major depressive disorder is 200 milligrams).
After a few months on Zoloft, my outlook on the world had improved dramatically. It sounds cliché, but my senses felt stronger. I noticed the colors on the cherry blossoms that spring. I actually had an appetite for food, and I appreciated the lyrics to my favorite music. I could joke around with my friends again. I began re-engaging in hobbies I had lost interest in, like tennis and theater.
Things seemed to be going well for a couple of years, but antidepressants can be precarious—when they work, they trick your brain into thinking you don’t need them anymore. By my junior year, I had taken myself off my medication cold turkey, not under the supervision of a doctor. This was not the smartest decision; I constantly felt lightheaded and got headaches, but I was convinced I didn’t need my medication anymore. And I actually did pretty well without them. Until I got to college.
Alone and Unwell
After a pretty dramatic breakup with my high school boyfriend during the first semester of freshman year, I had fallen back into my old patterns: sleeping constantly, procrastinating homework and avoiding assignments, and forcing myself to get out of bed to complete even the most basic of tasks. I white-knuckled my way through college without any sort of medication intervention.
Away from home and on my own for the first time, I wasn’t even sure how to go about asking for help or articulating what exactly was wrong with me. I was worried the services on campus wouldn’t be adequate; the running joke was that the student health center didn’t do much beyond asking, Are you sure you’re not pregnant?
After disastrous freshman and sophomore years, I ended up having to retake classes every summer to get my grades up and get into the journalism program, and I had to attend undergrad for a fifth year. While my mood had improved by then, I couldn’t figure out why I was still pushing off assignments until the last minute and ignoring emails—and why I couldn’t sit down to focus for more than 20 minutes at a time.
Once I graduated, everything was great…on paper. I had a solid relationship with my long-term boyfriend, a supportive family, and steady work in New York City, where I’d always dreamed about living. And yet, my depression crept back again. I noticed this pattern happening during major life changes—everything felt dark again, and I couldn’t navigate through the fog.
I worked to sustain relatively healthy habits, including going to the gym most days, eating plenty of vegetables, sleeping seven or eight hours a night, and maintaining an active social life. But no matter how hard I tried, I couldn’t shake the hopeless, helpless way I felt, and I still couldn’t bring myself to focus.
By age 27, I had gotten engaged and was planning a wedding when I noticed a strange pattern with my moods and thoughts. Some days I would feel so depressed and in such a bad, irritable mood that I could barely have a conversation with someone. I would often stay in the office until 8 or 9 p.m. just to complete my work, having spent most of the day incredibly distracted and unable to stay on task. Then, a few days later, I would get a creative burst or sense of euphoria; I had tons of energy, my thoughts were clearer, and everything felt bright and sunny again.
But eventually the darkness would reappear. I knew I had to get medical intervention, so I clicked through Zocdoc for a psychiatrist who took my insurance. After listening to me describe my symptoms and history with depression, he prescribed a low dose of Wellbutrin. This was the “it” antidepressant of the mid-2010s, and I had heard anecdotally how well people had done on it.
More Than Depression
After a few days on Wellbutrin, it kicked off what I now know is hypomania: I would stay up all night working on craft projects and could run on barely any sleep—then I would crash back down. My psychiatrist suggested the reason for this behavior was because things were going well in my life, but I knew this wasn’t the case. The only thing that had changed was this new prescription.
I had Googled my way into believing I had bipolar 2, which is a milder form of bipolar disorder where you experience episodes of hypomania rather than the full-blown manic episodes of bipolar 1. When you’re hypomanic, you have more energy and more creativity and feel euphoric; at the sake of downplaying a serious mental illness, hypomania feels pretty damn good.
Until it doesn’t. Your thoughts race so quickly, you can’t pin one down. Your judgment is slightly impaired, and you become more impulsive; dropping hundreds of dollars online seems like a fabulous idea because you need a whole new wardrobe right this moment. After days in a depressive funk, this feels like a welcome relief. But just as fast as hypomania comes on, it flees, sending you back to a depressive state.
I decided to see a new psychiatrist who could treat my suspected bipolar disorder. After describing my symptoms, he prescribed me Equetro, an anticonvulsant used to treat seizures and bipolar (for mania and mixed episodes). For bipolar, most docs pair Equetro with a mood stabilizer or antidepressant, but mine said we’d check in a couple weeks to determine whether I needed that extra Rx.
We never made it that far. Equetro made me feel like a zombie, and my depression was worse than ever. Every morning, I felt like I had gotten hit by a truck, and I had to peel myself out of bed just to brush my teeth and dry-shampoo my hair before work. My psychiatrist wasn’t returning my frantic calls, so I again took myself off medication, because I didn’t know what else to do.
My next psychiatrist, a woman whose office was filled with woodland fairy trinkets, prescribed me Latuda, an antipsychotic that helps with schizophrenia and bipolar depression—but nothing for my mood fluctuations, hypomania, and irritability. She never explained this decision.
I was running out of options, but I happened to find another psychiatrist who took my insurance, and he actually seemed to believe me when I explained my symptoms and suspected bipolar 2 diagnosis. He kept the Latuda, but paired it with lamotrigine, the generic form of Lamictal, which is a mood stabilizer used to treat seizures and bipolar disorder.
After a couple of years on the Latuda + lamotrigine combo, I was doing well and felt stable. Then, after I landed my dream job, I was hit with debilitating anxiety and horrific intrusive thoughts. The thoughts would play on a vivid loop in my head from the moment I woke up until I went to sleep. My heart would race, and I couldn’t think of anything else. This went on for two full weeks, and it was akin to torture.
Armed with a new job and new insurance, I found yet another psychiatrist who did an intake assessment. We kept the Latuda and lamotrigine, and I saw the physician’s assistant for medication management. His solution—during the approximately five minutes we met in person each session—was to titrate up the lamotrigine, since this doctor’s office didn’t prescribe benzodiazepines, such as Xanax or Klonopin, which are often used to reduce acute anxiety. I hoped the higher dose of lamotrigine would do the trick.
I knew I should see a therapist in addition to a psychiatrist. Medication can only do so much, and I needed help managing my negative thought patterns. I had a tough time finding someone who took my insurance, that I clicked with, or who would even show up to our appointments (I got ghosted twice with zero apology).
OMG, Now ADHD?
Three years into the job, I was having trouble paying attention and staying on task, leading to a couple poor performance reviews and mounting stress. I began to suspect I had ADHD. It explained the symptoms I had experienced my entire life: easily distracted, poor time management, procrastination, forgetting important details, losing papers, starting projects and never finishing them.
GOTTA READ: Is It ADHD? Bipolar?? Or Both???
Stimulants like Adderall and Vyvanse are typically prescribed for ADHD, but my psychiatrist’s office at the time also didn’t touch stimulants. (I learned it isn’t uncommon for some psychiatrists to avoid benzos and stimulants, as both drug classes have a high misuse and abuse rate.) When I told the physician’s assistant I was struggling with feeling distracted and scatterbrained, he wrote me a script for atomoxetine (brand name: Strattera) minutes later—no intake or assessment.
You can probably see where this is going: Atomoxetine did nothing for me. My work and quality of life were getting so awful, I talked to HR about going on short-term disability leave for my mental health. It wasn’t until a particularly negative Zoom meeting with my manager, where I popped a blood vessel in my eye during a fit of sobs (in the middle of a global pandemic, no less), that I decided I’d pay whatever premium was necessary to see better professionals who took more than five minutes to actually hear me.
I found a therapist in my neighborhood who seemed promising. After a couple sessions where I detailed my lifelong experience of what I assumed was undiagnosed and unmedicated ADHD, and how I’d spent decades masking my symptoms, she said, Ok, so psychiatry ASAP.
She referred me to a top psychiatrist who charges $500 a session, but I was desperate. During our telehealth appointment, this psychiatrist was different—patient, understanding, and attentive throughout our 30-minute appointment. He asked careful questions, then sent a six-page questionnaire so he could assess my ADHD symptoms.
At a follow-up, he agreed that I did, in fact, have ADHD, and he prescribed the stimulant Vyvanse. Since the Latuda and lamotrigine had been working to treat my depression and hypomania symptoms, he kept me on that combo but insisted I let him know if I experienced any adverse reactions to the Vyvanse. (It’s been known to trigger hypomanic episodes.)
So Many Barriers, So Much $$$
It’s been 18 months, and this trio of prescriptions is working well. I take my Vyvanse first thing in the morning, and it’s made a world of difference for me and my executive function. I can bring myself to complete basic tasks. I can focus on work in longer chunks. I procrastinate much less, I keep track of stuff better, I can nail down my thoughts, and I don’t have decision paralysis nearly as often.
Medication doesn’t make all my ADHD symptoms disappear, but it’s a useful tool. Before I got the official ADHD diagnosis and the stimulant prescription, I thought being easily distracted and forgetful was who I was as a person. Now I realize they are symptoms of a mental disorder and how my neurodivergent brain works. Turns out, I’m actually quite organized and type A, I just needed systems in place to keep me on task and manage my time and workflow.
I still take my Latuda and lamotrigine at night before bed, but I have worked with my psychiatrist to titrate my dosage down. I’ve begun to wonder if one day I’ll be able to come off mood stabilizers altogether: I can’t remember the last time I had a hypomanic episode, and I’ve only had a handful of depressive episodes over the past year and a half. But unlike in the past, I realize this means the medication is working how it’s supposed to.
In this country, quality mental healthcare is such a barrier, and for the longest time, I just assumed that professionals doing the bare minimum to treat you was the norm. Although it took additional research, work, and a lot of trial-and-error, I’m happy with the team I now have in place.
I honestly don’t know where I would be mentally and emotionally without my therapist and psychiatrist. I see my therapist every other week, and my psychiatrist every three to six months, though he’s reachable via text at all hours of the day, every day of the week, if I have questions or issues.
I was recently laid off from my full-time job in January, and the scariest part for me is losing access to good health insurance—which paid 80 percent of the costs of my expensive doctors. Without insurance, I wouldn’t have been able to get where I am with my mental health. My quality of life now compared to even two years ago is night and day.
MENTAL NOTE: A medication one person takes may not work for another and may have different side effects. Always talk to your doctor before trying or switching psychiatric medications.