It’s perfectly natural to experience a wide range of emotions—just peep one of those Feelings Wheels that keep popping up on your Instagram Discover page. But for the 45 million people worldwide with bipolar disorder, intense and abruptly changing moods color way outside the lines of the standard emotional spectrum.
What’s Bipolar Disorder?
Previously known as manic depression, bipolar disorder is a mental health condition that’s characterized by extreme mood swings, i.e. episodes or cycles, between depression and mania. It’s a lot of words to understand, especially if you just got a diagnosis, so let’s break it down…
Depression: We’ll get into the specific symptoms of this later, but bipolar depression is similar to the kind of depression you likely know about—you’re not into the stuff you used to love, your motivation is at zero, you find yourself getting irritable or teary at small things or for seemingly no reason at all.
Mania: Sometimes called a high, mania doesn’t mean you’re simply happy or upbeat. Think of it more like frantic or intense energy—like you had one (or five) too many espresso shots. You might actually feel amazing, even invincible, but you may also do things you’d never typically do and can end up regretting. (More below.)
Mood swings: Also known as episodes or cycles, they’re defined by how much time you spend in a state of depression or a state of mania. Depending on the type of bipolar you have (yes, it gets more complicated), these episodes/cycles/swings can be drawn out or just a blip.
The length and frequency of bipolar episodes can also vary greatly between individuals, but they could last mere hours to months. “With bipolar, you can have weeks of sadness or indifference, followed by a flurry of impulsive behavior that sometimes becomes psychotic,” says Ami Baxi, M.D., a psychiatrist at Northwell Health in New York City, adding that psychosis can manifest as delusions, hallucinations, or other breaks from reality.
We Mentioned There Were Types of Bipolar Disorder…
Bipolar disorder actually isn’t one disorder—it’s several.
- Bipolar I: This is the most common, and involves episodes of both mania and depression, with manic episodes lasting at least seven days or requiring hospitalization.
- Bipolar II: This type doesn’t extend to full mania. Instead, it’s predominantly marked by depression and hypomania—a milder, more fleeting form of mania.
- Cyclothymic disorder or cyclothymia: Milder forms of both mania and depression. According to the Mayo Clinic, this is considered relatively rare, and symptoms may be intermittent enough that medications are not used. (More on that later.)
- Unspecified bipolar: When someone doesn’t meet the criteria for the other three types, they’re categorized as unspecified. This involves having periods of unstable moods, but not to the degree that it warrants a diagnosis of bipolar I or II.
What are Some Symptoms of Bipolar Disorder?
They’re broken down by the two sides of bipolar.
The Depressive Symptoms
- Extreme fatigue
- Sleep issues, such as sleeping too much or insomnia
- Significant weight changes
- Feeling hopeless and worthless
- Suicidal ideation
- Loss of interest and pleasure in activities you once enjoyed
- Tendency to withdraw and isolate
The Manic Symptoms
- Impulsivity, including heightened promiscuity, substance use, and risk-taking
- Exaggerated sense of self-confidence
- Abnormally upbeat and “wired”
- Little sleep, if any
- Extremely talkative
- Easily distracted
It’s important to note that bipolar disorder often shows up when you’re young, with symptoms beginning as early as the pre-teen and teen years, says Anandhi Narasimhan, M.D., a clinical psychiatrist and neurologist in Los Angeles. This can make it hard to distinguish between what’s a symptom of bipolar disorder and what’s a symptom of…life.
“When you’re young, especially as a teenager or young adult, your life is changing in dramatic ways, so you may feel unstable in general,” says Dr. Narasimhan. “Moods may be up and down, you have sleep disturbances, and you’re more irritable, which can all look an awful lot like just dealing with normal life shifts.”
GOTTA READ: On the Spectrum: A New Way to Look at Bipolar
When those highs and lows begin to get more pronounced, however, then it’s time to talk to a health professional— especially if it’s messing with your normal functioning.
Why Do I Have This? What Causes Bipolar Disorder?
There isn’t a single cause of the condition, but there are several factors that increase your risk of developing bipolar disorder. These include:
Genetics
Most health conditions—mental or otherwise—are greatly impacted by your genes. Bipolar is indeed aa family affair, with research suggesting that you risk of developing it jumps ten-fold if someone in your immediate family has the condition. If one parent has bipolar disorder, there’s a 10 percent chance that their child will go on to develop it.
Sex
The condition affects slightly more women than men, according to a meta-analysis published last year in the International Journal of Bipolar Disorders. One theory as to why: reproductive hormones, says Dr. Baxi. This would explain why symptoms often worsen during hormonal shifts like menopause, when estrogen levels decline.
Pregnancy
On the topic of hormones and oh God not another thing pregnant women have to deal with… Because the incidence of bipolar disorders in women peaks during reproductive years, it often manifests (or worsens) during pregnancy. Research shows that the stress of pregnancy and childbirth can trigger the disorder for the first time and exacerbate pre-existing bipolar symptoms. Pregnant women or new mothers with bipolar disorder have seven times the risk of hospital admissions compared to pregnant women who do not have bipolar.
Identity
LGBTQIA+ populations are at heightened risk for mental health conditions—including bipolar disorder—which researchers attribute, at least in part, to increased adversity. According to the National Institute of Mental Health, 4.4 percent of adults experience bipolar in their lifetime, but 7 percent of bisexually identified men and women reported the condition in a small 2017 survey.
Race
Bipolar doesn’t seem to occur more in one race than another, but research does show disparities in terms of care. Studies have found that Black patients are more likely to be misdiagnosed with another condition, like schizophrenia, and given less intensive treatment than white patients.
How Bipolar Disorder Affects Work, Love, and Friends
Work and relationships can take a major hit, says Dr. Baxi, particularly in the throes of a manic or depressive episode. Even mania—a so-called high—might leave someone feeling too restless or impulsive to show up to work, and Dr. Baxi says any degree of stress can trigger or deepen an episode.
That’s why project manager Shannon Vought found it tough to maintain a job even when the duties seemed reasonable. “At one point, the president of the company where I was working reached out to me directly and said they were putting me on leave,” she recalls. “Just after my 30th birthday, when I had a good job and a fiancé, I was sitting in a psych ward trying to learn coping strategies.”
That might sound disheartening, but Vought believes it saved her life. While in the hospital, she was put on different medication, and also started a new treatment plan that combined therapy with education on stress reduction and building a stronger support team. Even just learning to take a walk every day gave her more structure and built a healthy habit. “I’m on such a better track and I have a new job that’s going great because I learned how to be more in control,” she says.
The Best Treatments for Bipolar Disorder
There isn’t a gold standard treatment for bipolar disorder, says Dr. Narasimhan, simply because there’s such a wide variation among individuals when it comes to intensity of symptoms, duration, onset, and progression. According to the National Alliance on Mental Illness (NAMI), treatments can include both medications and other mood-management strategies. This might mean a mix of:
Cognitive Behavioral Therapy (CBT)
This is a type of therapy, often used in conjunction with meds, that teaches you coping skills and has been found to help decrease depression symptoms, mania severity, and the relapse rate for bipolar episodes (a relapse means when you experience depression or mania again after you haven’t for a while).
Complementary Treatments
Education on self-management and coping strategies—such as techniques for lowering stress, getting quality sleep, and eating healthy—and mindfulness, which can support (but not often replace) medication and psychotherapy.
Medications
- Mood stabilizers like lithium (Lithobid) strengthen nerve cell connections in parts of the brain associated with mood regulation, which can help reduce depression a and mania for those with bipolar
- Antipsychotics like aripiprazole (Abilify) affect dopamine receptors in the body; these neurotransmitters play a role in motivation and reward, and some research suggests dopamine regulation can have a significant effect on bipolar disorder.
- Antidepressants like fluoxetine (Prozac) are used in treating bipolar depression and are often paired with antipsychotics to keep those with bipolar from swinging too far in either direction.
Medications can take time to adjust and, adds Dr. Narasimhan, some people may require all three main types of meds, while others with milder bipolar II may only need mood stabilizers. One difficulty she often sees is that when people feel better after starting medication, they may take it as a sign they don’t need it anymore, stopping abruptly. This is a huge problem, says Dr. Narasimhan, because stopping in this way increases the risk of having a psychotic episode.
What’s key to any treatment for bipolar is having a great doctor or doctors, typically a psychiatrist and possibly also a psychologist—a primary care doc doesn’t have the s specific training to properly help you manage this condition (though they can recommend a specialist if you need a recommendation). And also: Make sure they’re just as good of people as they are medical pros. You want to feel as comfortable as possible opening up about things.
How Bipolar Disorder Feels, According to Women Who Have It
“I would be doing fine for a while with a good job, relationship, and support system and then a darkness would overtake me and I couldn’t get off the couch. I didn’t have a plan for suicide, but often wished I could get in a car accident so I didn’t have to live this way anymore.” —Shannon Vought, 30, a project manager in North Carolina
“Every few months, I had a new life plan. I was going to change my major and become a math teacher, then I was going to learn Russian and work for the foreign service, and on and on. I’d be awake for days, excited that I’d finally figured out my life, and then crash, hard, and hide in my dorm room.” —Michelle Reittinger, 47, Utah-based developer of My Upside of Down, a program that focuses on integrated approaches to addressing bipolar disorder
“Before medication, there would be rapid cycling between excess energy and a downward spiral. When you’re in it, and trying to run away from every emotional fluctuation, you never think you could have harmony in your life. It took a long time to integrate more practices like meditation and journaling that could allow me to sit with my feelings and not have them dominate my actions.” —Marisa Imôn, 35, a writer in Vermont
3 Things You Should Not Say to Someone With Bipolar Disorder
You’ve got a friend or family member with bipolar, and it’s only natural you want to help. But sometimes well-meaning support can backfire. Case in point? These three phrases that end up sounding tone-deaf to someone dealing with bipolar.
1. “You should get more exercise.”
Yes, there’s plenty of research suggesting that exercise can have a beneficial impact on mental health, particularly depression and anxiety. But this suggestion often makes it sound like you can resolve a disorder just by going for a run, according to Dr. Baxi.
Instead, say… “Want to go for a walk with me?” Often, support is simply being there, literally, and getting active together can show that.
2. “I can relate—I’ve been feeling bummed out lately, too.”
Even if you’ve been diagnosed with depression, or have depressive symptoms, it’s not the same as bipolar disorder. Many with the condition already feel like no one understands them, says Dr. Narasimhan, and a phrase like this will reinforce that belief. Plus, it sounds dismissive, like their condition is just the weather, not the climate in which they live all the time.
Instead, say… “I don’t know what it must feel like to go through what you do. Did you want to talk about it?” Acknowledging that you can’t relate, but you want to understand, can go a long way.
3. “It’s good to see you so happy. I hate seeing you sad.”
Women already struggle with societal expectations of the way we’re supposed to act. (Cue: “Hey, you’d be prettier if you smiled.”) And those with bipolar feel this down to their bones. Even at age 10, Marisa Imôn remembers trying to “play happy” because she saw how disapproving her family and others could be when she was withdrawn and sad. Phrases like these imply that being upbeat is the only healthy way to be, which puts more pressure on someone with bipolar.
Instead, say… “How are you feeling today?” That’s it. Just check in and let the answer stand.
Bottom line: “What’s important when someone is struggling is that they know there’s someone they can trust—that’s essential for bipolar,” says Dr. Narasimhan. “This is a condition that is helped by a strong support team, so whether you have bipolar and are building that for yourself, or you’re family or friends with someone with the condition, you have to get in the mindset of addressing this together.”
Related Conditions to Bipolar Disorder
Don’t want to overwhelm you, but it’s important to understand that having bipolar disorder has a been linked with other mental health conditions, too: The National Comorbidity Survey found that 95 percent of bipolar respondents met criteria for three or more psychiatric disorders. But because bipolar is so complicated, it’s also frequently missed or misdiagnosed.
Anxiety
A long-term study from the National Institute of Mental Health—called Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD)—found that the lifetime risk for developing an anxiety disorder in addition to bipolar disorder is 51.2 percent, tending to affect bipolar I and II types more than others.
ADHD
In a 2021 study, around 10 to 20 percent of adults with bipolar also had ADHD. There’s also symptom overlap between the two conditions: mainly, impulsiveness and the inability to relax.
Personality Disorders
A recent study found personality disorders including borderline, narcissistic, antisocial, and histrionic appear in a third of bipolar patients.
Cardiovascular Disease
You may think “isn’t that an old man’s disease?” But data has found increasing rates of heart attack in younger women. Cardiovascular mortality is almost twice as high in patients with bipolar disorder, which may be related to an increase in factors like smoking, diet, and sedentary lifestyle.
Psychotic Disorders
Because severe cases can sometimes present as psychotic episodes, bipolar disorder can be misdiagnosed as schizophrenia or a schizoaffective disorder (and vice versa). But research shows that the three conditions share some genetic components and can indeed coexist. Per a Danish study found, a female bipolar patient’s risk of also being admitted with a schizoaffective disorder by the age of 45 was approximately 103 times higher than that of a woman at the same age in the general population.
Depression
Because the lows are so distinctive and the highs might be fleeting, bipolar disorder is often mistaken for clinical depression, says Dr. Baxi. That’s particularly true if manic periods are short or infrequent. Sometimes, however, depression is predictive of bipolar disorder. In a large population-based study, around 8.4 percent of patients with major depressive disorder—a severe form of depression—went on to be diagnosed with bipolar disorder.
Where Can I Find Help for Bipolar Disorder?
The Orgs
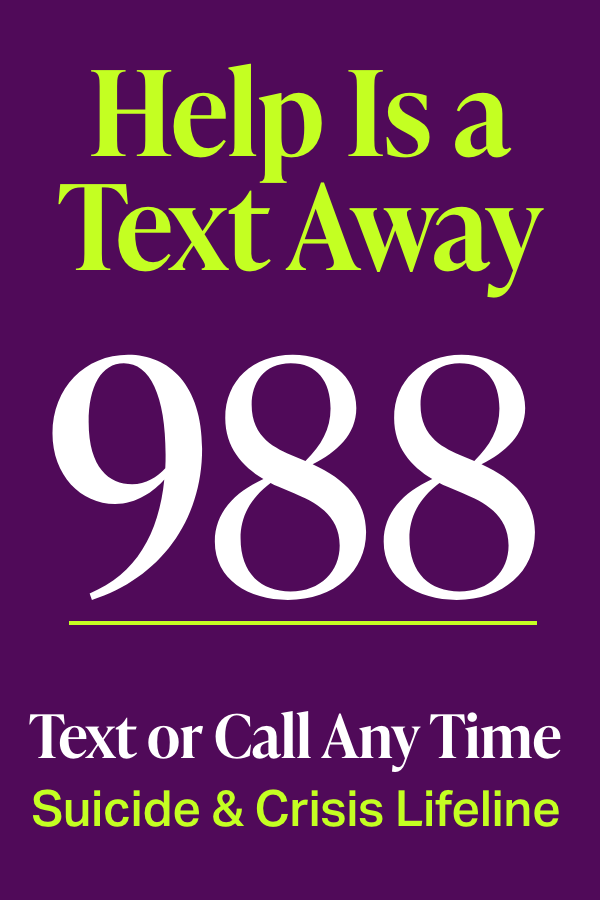
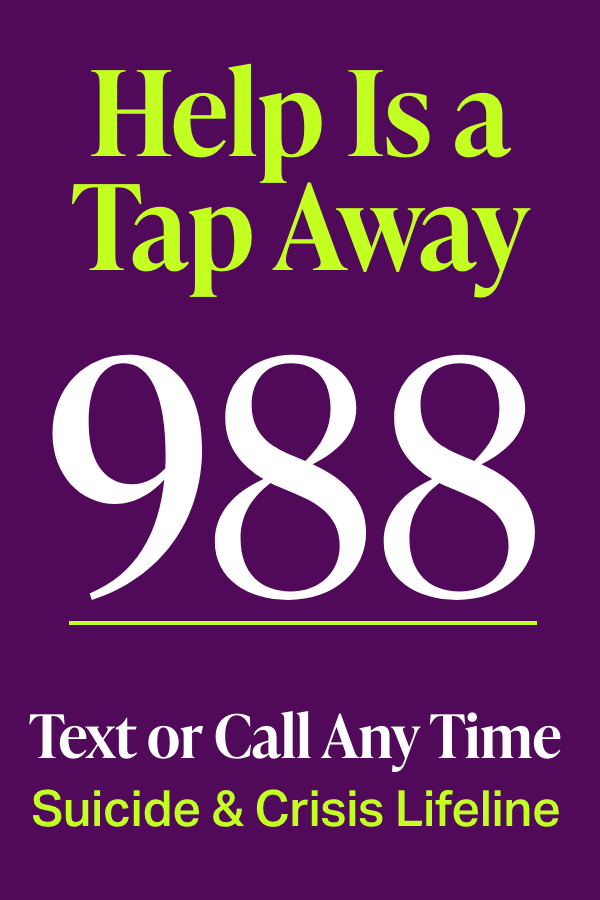
National Alliance on Mental Illness (NAMI). NAMI offers resources, research links, support, and a two-part podcast series on bipolar disorder. Call the helpline at 800-950-NAMI or start an online chat. If it’s a crisis, text “NAMI” to 741741.
American Psychiatric Association. Search their database for a mental health professional based on location and specialty, because the right doctor—one who knows bipolar well—is so important.
Depression and Bipolar Support Alliance. Listen to their podcast series I’m Living Proof: A Letter to My Younger Self, which offers real stories from people struggling with bipolar disorder.
The Follows
The upside of social media—it’s given a voice and a platform to real people living and dealing with all sorts of mental health conditions, minimizing a once-blaring stigma. These bipolar disorder advocates are particularly inspiring.
@the_bipolar_barbie
Follow because: An artist whose ink drawings often depict what it’s like to deal with bipolar. She also has two super cute dogs.
Angel, @angelfromthebloc
Follow because: This TikTok-er chronicles daily life with bipolar, including issues like manic spending and addiction.
O, @bipolar_2_life
Follow because: Certainly has a knack for finding and creating bipolar-themed memes, while also raising awareness about the importance of staying visible if you have bipolar.
The Apps
Michelle Reittinger says doctors wanted her to keep a journal to track her moods, but she felt overwhelmed by the blank pages. She found that using an app was much easier and helped her keep an eye on her emotional trends. She uses Bearable, but other options include eMoods, Mood Log, and MindDoc.
Bipolar Prevalence: Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. The Lancet. November 10, 2018.
Cyclothymic Disorder: Cyclothymia (Cyclothymic Disorder). Mayo Clinic. December 13, 2022.
Brain Structure and Function: Bipolar Disorder. National Alliance on Mental Illness. August 2017.
Prevalence in Women: Arnold L. Gender Differences in Bipolar Disorder. Psychiatric Clinics of North America. September 2003.
Race: Johnson K, Johnson S. Inadequate Treatment of Black Americans with Bipolar Disorder. Psychiatric Services. February 1, 2014.
LGBTQIA+: Kidd S, Howison M, Pilling M, et al. Severe Mental Illness in LGBT Populations: A Scoping Review. Psychiatric Services. February 29, 2016.
CBT and Bipolar Disorder: Chiang KJ, Tsai JC, Liu D, et al. Efficacy of Cognitive-Behavioral Therapy in Patients with Bipolar Disorder: A Meta-Analysis of Randomized Controlled Trials. PLoS One. May 4, 2017.
Bipolar and ADHD: Virginio Salvi, Enrico Ribuoli, Michele Servasi,et al. ADHD and Bipolar Disorder in Adulthood: Clinical and Treatment Implications. Medicina. May 2021.
Comorbidity (1): Paul T, Javed S, Karam A, et al. A Misdiagnosed Case of Schizoaffective Disorder With Bipolar Manifestations. Cureus. July 28, 2021.
Comorbidity (2): Sagman D, Tohen M. Comorbidity in Bipolar Disorder. Psychiatric Times. March 23, 2009.
Comorbidity (3): Laursen T, Agerbo E, Pedersen CB. Bipolar Disorder, Schizoaffective Disorder, and Schizophrenia Overlap. Journal of Clinical Psychiatry. July 16, 2009.
Colliver V. Heart Attacks Striking Younger Women. Johns Hopkins Medicine.