One of the most memorable onscreen birth scenes (for this ’90s-era teen, at least) was on a 1992 episode of Murphy Brown. Candice Bergen’s character had just given birth to her son and was giving him a very Murphy-esque speech about the shortcomings he should expect from her as a mom. Then, in a hushed tone, she launches into a ponderous version of “You Make Me Feel Like a Natural Woman” while staring longingly into the baby’s eyes. Cue waterworks.
If our collective perceptions of birth are shaped in part by cultural moments, it’s easy to see why those perceptions may often be, well, skewed. Because reality is not a TV show.
The experience of birth as something natural and beautiful—as it is so often culturally rendered and upheld by many a mommy influencer on social media—is not universal or even all that common, says Paige Bellenbaum, LMSW, founding director of The Motherhood Center in New York, which specializes in treating pregnant and post-birth moms who have perinatal or postpartum mood and anxiety disorders (PMADs).
For months after the birth of her son, now 5, Arielle Moody was shrouded in a heavy fog. “I didn’t have any friends that had openly talked about postpartum depression [PPD], so I was unprepared for what I felt,” says Moody, co-founder of beauty brand Mama Sol. Extreme sleep deprivation and a self-imposed pressure to breastfeed made the situation more challenging. “I thought PPD had to be severe depression, and I didn’t feel like mine was severe enough to qualify, but it still absolutely affected me.”
The stories that dominate the news cycle don’t help with that distinction, since they tend to focus on the more singular cases of women whose drastic actions result in Dateline-special-level tragedy (see: the recent cases in Massachusetts and Maine). “Oftentimes, the press, unfortunately, misrepresents the diagnosis in these stories and refers to it as postpartum depression,” says Bellenbaum, explaining that these are examples of postpartum psychosis.
The latter diagnosis occurs in only 1 in 1,000 births and is a true medical and psychiatric emergency, says Lucy Hutner, M.D., a New York-based reproductive psychiatrist. Postpartum psychosis is a rare occurrence in comparison with PPD which, according to a recent study, happens in up to 19 percent of new mothers. And evidence shows that, during the height of the COVID pandemic, the rate of women citing depressive symptoms after childbirth shot up to 35 percent.
A challenge for Moody, and for a great many new parents, is distinguishing between feelings that might be considered “normal” versus those that would be deemed by a professional as “clinically significant.” The diagnostic criteria for postpartum depression is the same as for regular depression, just that it occurs specifically within the postpartum period (typically about four weeks after giving birth). “The most common symptoms that reflect a major depressive episode are really persistent low mood, low energy, poor concentration, some negative rumination, and sometimes feeling very guilty and like everything is your fault,” says Dr. Hutner.
But PPD can also come with symptoms you might not immediately equate with depression, such as prolonged irritability, intense agitation, and an edginess or short fuse. There can also be rage—something Bellenbaum says rarely gets highlighted but many new mothers feel. “It’s one of those emotions or symptoms that women feel so ashamed to talk about because what kind of mother would feel so angry all the time,” she says.
Lots of Acronyms, Lots of Overlap
As a topic, PPD has reached a level of hashtaggable popularity, it is postpartum anxiety (PPA) that is more widely present—and can often cause more of an impact.
Providing a clear definition of postpartum anxiety can be surprisingly hard to do. In part, that’s because some degree of hypervigilance and worry is normal, particularly since the brain changes during pregnancy. “There’s a very strong protective sense that comes out, so our job is to differentiate that from clinically significant anxiety, which is a totally different thing but also really common,” says Dr. Hutner.
Pinning down PPA can also be tricky because anxiety-related symptoms in the postpartum period can take so many different forms, from generalized worry to panic to obsessions. And the high comorbidity between PPA and PPD creates more confusion. “Depression and anxiety mingle with each other in the perinatal period at least 80 percent of the time,” says Dr. Hutner.
One way that doctors differentiate typical (but still stressful) anxiety from PPA is when a birthing parent can’t turn off their anxious thoughts—often referred to as intrusive thoughts—which become like a fast-moving train that sends them into a panic. How these play out: A new mom is both incredibly fearful of harm coming to their baby and also of being the cause of that harm. Bellenbaum recounts women sharing that they’re afraid of getting near the stairs because they worry that they might throw the baby down them, or fearful to go in the kitchen and be near the knives because one might accidentally jump into their hand and stab the baby.
If you’re shocked, we’re not surprised. Thanks to stigma, people barely speak about this beyond a whisper. But know this: Intrusive thoughts post-birth are widespread, and when they are not accompanied by psychosis—which, we repeat, is extremely rare—they are considered ego-dystonic. In other words, these thoughts are antithetical to your core beliefs. That’s why they are called “intrusive.” They are unwanted.
How can you tell the difference between intrusive thoughts you’d never act on, and an emergency situation? Some of the most distinctive qualities of psychosis, says Bellenbaum, include:
- being out of touch with reality with fixed false beliefs (meaning: no amount of evidence can convince you something is untrue)
- experiencing hallucinations and delusions
- receiving auditory commands and hearing voices
- having jumbled speech and disorganized thoughts
- something called waxing and waning, where a person can go from making sense to, in a snap, appearing comatose
Most women are hesitant to share intrusive thoughts even with clinicians at The Motherhood Center until they’re directly asked. “When I tell you the look of relief that comes across the face of a new mother who is told that what she is thinking does not mean that she’s a bad mother, it’s huge,” Bellenbaum says.
Another big indicator of clinically significant postpartum anxiety? Persistent obsessions and compulsions that start to take over a new mom’s thinking. “I have patients who will say, I put the baby down and I tried to go to sleep but I ended up ruminating for hours and having to repeatedly go in and check on them,” says Dr. Hutner. “And then, even if they did fall asleep, they would wake up very, very anxious about the well-being of the baby.”
A Different Kind of PTSD
Our meme-loving, TikTok-y world has turned the words “trauma” and “traumatized” into everyday lexicon, often re: situations that are utterly non-traumatizing. Like, the barista made you a flat white instead of a cappuccino.
In fact, people are often more likely to throw the word “traumatic” around regarding a casual interaction versus PTSD from birth trauma, a significant postpartum mental health issue that is broadly overlooked and underserved. Depending on which report you believe, between 3 and 45 percent of new moms experience a traumatic birth experience, a chasm that may reflect how many women keep quiet about it. Perhaps, again, because of that collective “birth is beautiful” narrative we’re force-fed from so many forks.
As a study in The Journal of Perinatal Education discovered, new moms often don’t have the language to describe what they’re going through. “They feel like this is just how it’s supposed to go,” says Bellenbaum. In “Having a Baby After a PMAD,” the most successful group she runs at The Motherhood Center, every woman in the current session experienced birth trauma during the pandemic.
PTSD from birth trauma can result in a number of symptoms, including extreme anxiety, particularly around returning to stimuli that activates the trauma (like going back to the hospital where you delivered); distressful flashbacks; and frequent wake-ups and insomnia.
“What’s so unfortunate about PTSD from birth trauma is when we don’t talk about it, it doesn’t exist,” says Bellenbaum. “And as we all know, as soon as the baby is born, all the attention is on them, so often women are forced to hold that trauma deep inside. They are not given permission, nor do they feel as though they deserve permission, to talk about what their experience was like.”
What’s important to remember is that feeling trauma from your birthing experience is worthy and valid, even if it’s not as “bad” as someone else’s. At The Motherhood Center, the experts often repeat the expression that “trauma is in the eye of the beholder,” meaning what feels traumatic to someone is entirely subjective, and often influenced by a past history of trauma (including physical or sexual abuse) and other mental health conditions.
Getting Through It
At The Motherhood Center, it’s very common for their new and expecting mothers to present with moderate to acute perinatal anxiety disorder and have depression lurking underneath. Antidepressants remain an effective, oft-prescribed option for treatment.
While some providers are quick to tell women to go off these medications during pregnancy and postpartum, there are a number of safe antidepressants for women to take in the perinatal period, even if breastfeeding. The key, says Bellenbaum, is to be evaluated by a reproductive psychiatrist who can steer you to the appropriate medications.
As for therapeutic interventions, Bellenbaum points to cognitive behavioral therapy (CBT), which helps hone the skills to interrupt negative thinking patterns, and dialectical behavioral therapy (DBT), which trains women in how to make space for the entire span of emotions they’re experiencing. Your symptoms will help determine which type of therapy will work best (for example, people with obsessions and compulsions are better off with DBT than CBT).
“I often say to new and expectant mothers that you can both look at your baby and think they’re adorable and also feel like you’ve made the biggest mistake of your life,” says Bellenbaum. “And it doesn’t mean that you’re a bad mother. Just that you’re a human being with a complex range of emotions.”
To reduce anxiety in the moment, there are a number of effective exercises you can lean on. One that Bellenbaum suggests is holding something cold in your hand, splashing cold water on your face, or putting your head in the freezer (yes, really) because the temperature can help diffuse panicky feelings.
The positive news here, says Bellenbaum, is that we’re on the precipice of a maternal mental health boom, and there has been rapid growth in clinicians specifically trained to treat women with perinatal mood and anxiety disorders. “PSI (Postpartum Support International) now has a very specific certification and training that they offer to clinicians to get something called their PMHC (perinatal mental health certification),” explains Bellenbaum.
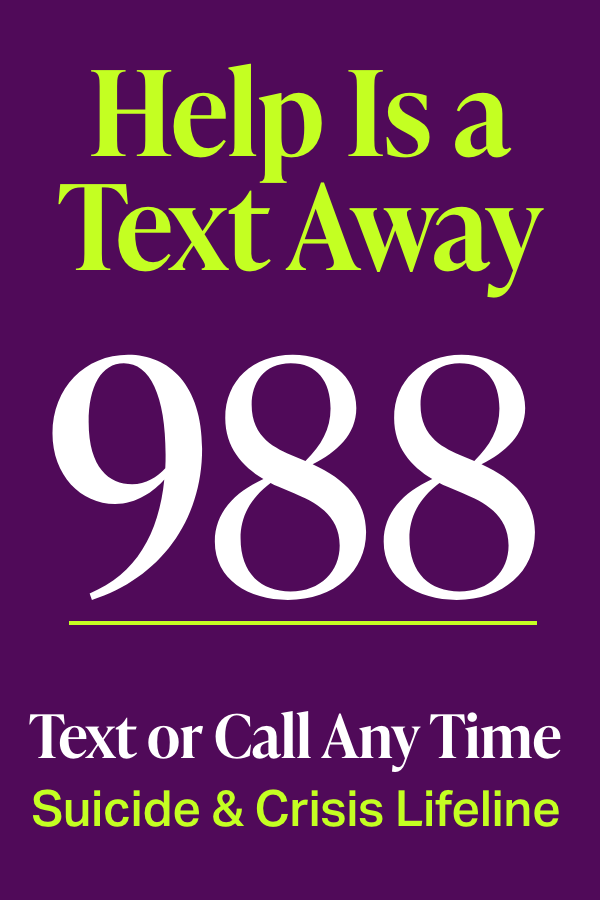
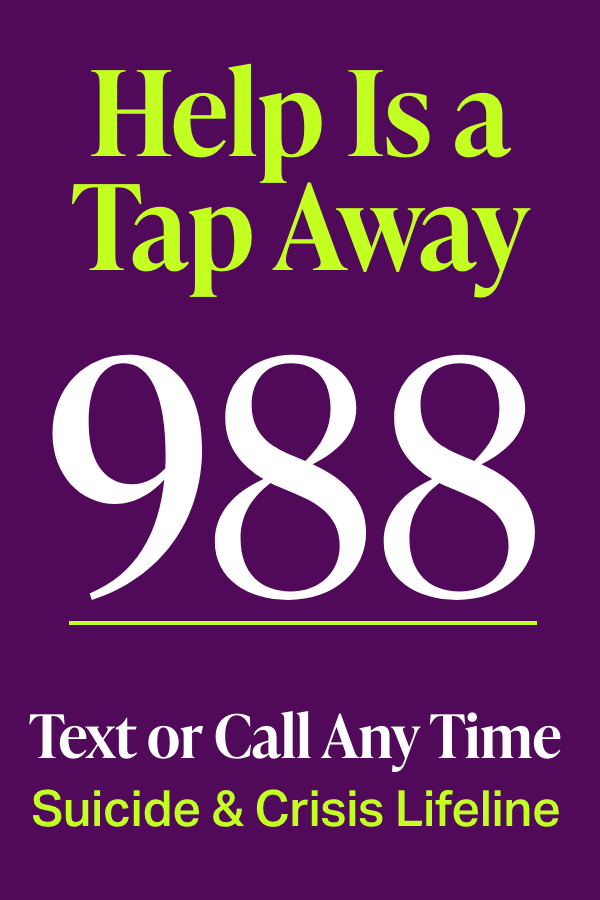
You can call or text 1-800-944-4773 (4PPD) to speak with a trained PSI counselor who can help you find a therapist and resources in your area; they’ll get back to you within 24 hours. If you need a faster response, you can call or text the new National Maternal Mental Health Hotline at 1-833-TLC-MAMA (943-5746), who will get back to you in a few minutes, any time day or night.
Sign up for our free newsletter
Legit tips and cool copes, delivered straight to your inbox.
By completing this form you are signing up to receive our emails and can unsubscribe anytime.
As for PTSD from birth trauma, experts say that the best way to both treat and avoid this is through trauma-informed care, where medical providers listen and engage in proactive communication with patients to forge a collaborative, supportive relationship. “There are incredibly effective ways to preserve a woman’s sense of control and autonomy in the birthing process,” says Bellenbaum.
A 2023 study published in Frontiers in Psychology utilized a self-assessment for new mothers who had experienced birth trauma. The study authors found that it allowed the women “to access their postpartum mental health status,” and recommended its use for “subsequent clinical applications” to provide better psychological intervention.
Dr. Hutner believes that having such a standardized screening process before birth could clue medical providers into their patients’ mental state, something that’s particularly crucial for Black and brown women, who experience more frequent medical trauma and have higher maternal mortality rates.
Shifting to trauma-informed care has a profound and positive impact. “It’s something we really need to take seriously in the medical community, because it can absolutely alter the overall outcome,” says Bellenbaum. Though trauma-informed care during the birthing process isn’t that common, experts say it should be the norm—and awareness is starting to grow.
For example, in an episode of Dead Ringers, the series where Rachel Weisz plays gynecologist sisters Elliot and Beverly Mantle, one sister handles a woman in labor who presents with previous trauma. “The woman didn’t want to be touched, she didn’t want to go on the bed, she didn’t want to be checked, and so the doctor turned around and said, I’m going to let you do all this, and coached her on exactly what to do,” says Bellenbaum, recalling the scene. “She completely and utterly gave power over to the woman in labor.”
For birthing people who are suffering with PTSD from not having that kind of care, trauma-informed care is also the best treatment. This involves active listening by a professional trained in treating trauma. (Postpartum Support International (PSI) is a terrific resource for finding help.)
Through the gradual process of being able to talk honestly about your trauma—and having your experiences validated—healing can happen, says Dr. Hutner. Addressing this kind of trauma is so important; left untreated, birth trauma can cause difficulties bonding with your newborn or breastfeeding, as well as severe anxiety symptoms, including fear or avoidance of going through childbirth again.
While seeking treatment, beware of therapists who promote “posttraumatic growth,” says Dr. Hutner. Though the term was first developed by psychologists Tedeschi and Calhoun in the mid-1990s, it’s buzzing around TikTok now. “My ambivalence about the phrase itself has to do with the fact that sometimes traumatized patients in my practice have well-meaning friends or family say things like, Things happen for a reason, which can inadvertently lead to minimization or self-blame for the traumatized individual,” says Dr. Hutner. “The intense difficulty of a traumatic event and things that allow us to grow are not always the same thing.” In other words: We shouldn’t have to endure trauma to grow.
She prefers to help mothers move forward by changing their narrative. “Sometimes the difficulty with trauma is that you feel so helpless, and you feel like you’re being acted upon,” she says. “My job is to try to help someone reframe that and point out the amazing way that they coped in the moment, and ideally that will translate into a greater sense of self-efficacy and agency.”
As with all health conditions, simply being more open—with a professional and even with each other—about the spectrum of perinatal mental health issues that naturally arise for so many women is a good step. Awareness leads to knowledge leads to less stigma and more treatment-seeking.
For Moody, what helped make her feel like herself again when she was experiencing PPD was a weekly gathering of mothers in her neighborhood. “It was absolutely everything for me,” she says. Community is, indeed, integral to the recovery process. Says Bellenbaum: “Being able to talk about it, share it, process it. Every time you’re able to revisit it, the less power and control it has over you.”
Read More About Mental Health and Pregnancy
Stats about PPD: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9851410/
Stats about PTSD from Birth Trauma: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6193358/
Study about Testing for Birth Trauma: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9970998/
Trauma-Informed Care Basics: https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562
Research on Trauma-Informed Care: https://pubmed.ncbi.nlm.nih.gov/34776109/
Study About Women’s Experiences of Birth Trauma: https://pubmed.ncbi.nlm.nih.gov/33020046/