There was a time in the late ’90s when real people struggling with a very real mental health condition were “talent” to entertain the masses. Sally Jessy Raphael, Jenny Jones, and other daytime talk-show hosts devoted multiple hour-long segments to eating disorders. Inevitably, they’d welcome to set a woman—always jaw-droppingly thin, always white—in the throes of her disorder. Her family members would appear, teary-eyed and desperate. This type of narrative dominated the media for years.
You’d think we’d have evolved more in the past 30 years, but in some ways we’ve simply relocated the tales to different platforms. Social media algorithms—even on the more-newsy Twitter—favor images of slim bodies, and “what I eat in a day” videos are all over TikTok.
Eating disorders remain an epidemic in this country. According to the National Association of Anorexia Nervosa and Associated Disorders (ANAD), an estimated 28.8 million Americans, or 9 percent of the population, will have an eating disorder in their lifetime. (By the way, that’s about the same as it was in the ’90s.)
This number is sure to be underreported, as many hide their eating disorder (ED). That’s particularly scary when you consider that over 10,000 people will die each year as a direct result of an eating disorder. These are preventable deaths, which is why awareness and early intervention are so important.
Here’s what else we know about eating disorders: They don’t just affect slim, white women. People from a racial or ethnic minority, or who are overweight, are actually at an increased risk. Between these outdated stereotypes and the rising incidence of EDs, we’re long overdue for a new, more nuanced conversation. So let’s talk (just not talk-show talk).
What’s the Difference Between Watching What I Eat and Having an Eating Disorder?
It can be hard to know when you’ve crossed the line—and a history of dieting does up your chances of developing an eating disorder, says Elizabet Altunkara, LMSW, the director of education at the National Eating Disorders Association (NEDA). However, dieting or tracking what you eat through calorie-counting apps doesn’t equal a diagnosable ED.
“An eating disorder is any eating pattern that significantly compromises physical health and emotional well-being,” says Debra Safer, M.D., an associate professor of psychiatry at Stanford University and the co-director of the Stanford Adult Eating and Weight Disorders Program. Eating disorders can have dire consequences. When you don’t eat enough, for one, your heart can become permanently damaged.
“Eating disorders are bona fide medical illnesses—just like diabetes,” says Charlynn Small, Ph.D., the assistant director for health promotion at the University of Richmond Student Health Center in Virginia and president-elect of the International Association of Eating Disorders Professionals Foundation.
One key sign your eating habits may have become disordered: not being willing or able to change them, even when a doctor advises it as medically necessary. An example: If you are at an unhealthy weight and your doctor tells you to eat more and exercise less “and you can’t, or it seems too frightening, then you’ve crossed over into an eating disorder,” says Dr. Safer. Now, it bears repeating, someone does not need to reach an unhealthy weight to have an eating disorder; people of any weight can have one.
There are telltale clues to an eating disorder, though not everyone will exhibit them. “Even though these are warning signs, it is important to note that it is best to see a professional and get help at the first sign of disordered eating,” Altunkara says.
In the broadest terms, these signs include:
- Weight loss, dieting, and control of food are a primary concern in your life
- Becoming socially withdrawn
- Experiencing extreme mood swings
- Noticeable weight fluctuations
- Difficulty concentrating or sleeping
- Issues with dental, skin, hair, and nail health
- Gastrointestinal problems
This list has a lot of “weight” in it. But eating disorders aren’t always tied to the desire to lose weight. EDs are complex beasts, and we use that word purposely. EDs are really hard on you—body and mind—so if you see yourself on this page, remember to treat yourself with compassion.
What Are the Types of Eating Disorders?
The main eating disorders are anorexia nervosa, bulimia nervosa, binge-eating, and a catchall category called other specified feeding or eating disorder (OSFED).
- Anorexia nervosa: This type of eating disorder is about proportion: It’s defined by restricting nutrient intake relative to nutritional guidelines. While this can lead to significantly low body weight, it’s not always the case. Though Sally Jesse, a slew of Lifetime movies, and unfortunately some 2023 media typically portrayed bodies with anorexia as looking a certain way, we’ve got two words: They don’t.
Anorexia shows up as humans show up—in every shape, size, and color. And no matter your weight, anorexia can be extremely detrimental to your health. Back to heart problems: One study out of the University of California at San Francisco found that people in larger bodies who have anorexia are just as likely to experience heart irregularities as underweight people with anorexia.
Although anorexia manifests through food restriction, a quest to be thin doesn’t always drive the behavior. “People often think that anorexia is about dieting and losing weight, but it’s more complicated than that. Oftentimes, eating disorders are not about food,” Altunkara emphasizes. “They emerge as a way to handle difficult emotions, and an attempt to regain control of a world in which the person has felt powerless.”
- Bulimia nervosa: Bulimia involves a cycle of binge-eating and purging. People with bulimia frequently eat large amounts of food in a short period of time, and don’t feel in control of their actions. They eat when they’re not hungry, and past the point of feeling full. Then, to counter this, they force themselves to vomit, use laxatives or diuretics, excessively exercise, or fast to lose weight. There’s usually a fear of weight gain and an intense unhappiness with their body image.
- Binge-eating disorder (BED): BED is similar to bulimia in that it involves loss-of-control eating that leads to feelings of shame, distress, or guilt. Unlike bulimia, the episodes are not followed by purging behavior.
- Other specified feeding or eating disorder (OSFED): This last ED category encompasses disordered eating patterns that don’t meet strict diagnostic criteria for anorexia nervosa, bulimia nervosa, or binge-eating disorder. (Very clear, we know.)
How Do I Know if I Have an Eating Disorder?
Eating disorders don’t spring up overnight like a big zit; they can develop slowly, over time, which makes them so insidious. “People who have eating disorders don’t even realize a lot of times that they are struggling with it because it’s such a progressive disorder,” says Bethany Crowley, CEDS, a certified eating disorder specialist based in Kailua, Hawaii.
An eating disorder can show up in so many ways—from mind to body to actions. If you look at the below list of symptoms and several are resonating, that’s a sign to reach out to a therapist or your healthcare provider. (You can also check in on yourself with NEDA’s eating disorders screening tool.)
Emotional and Behavioral Symptoms of an Eating Disorder
- Preoccupation with weight, dieting, or control of food
- Preoccupation with counting calories, carbohydrates, or fat grams
- Refusal to eat certain foods
- Discomfort when eating around others; eating in secrecy
- Food rituals (for example, eating only particular foods, chewing excessively, or not allowing foods to touch)
- Withdrawal from friends and activities
- Extreme concern with body size and shape
- Frequent checking in the mirror for perceived flaws in appearance (emphasis on “perceived,” because You. Are. Enough.)
- Excessive, rigid exercise regime—despite bad weather, fatigue, or if you’re sick or injured
- Feelings of disgust, depression, or guilt after overeating
- Frequent trips to the bathroom
Physical Symptoms of an Eating Disorder
- Noticeable fluctuations in weight, either up or down or both
- Stomach cramps or other gastrointestinal complaints (things like constipation or acid reflux)
- Irregularities with your period
- Difficulties concentrating
- Dizziness, especially when you stand up, or fainting
- Feeling cold all the time
- Sleep problems
- Cuts and calluses across the top of your finger joints (these can arise from induced vomiting)
- Dry skin and hair and brittle nails
- Swelling around the area of your salivary glands (just below your ears and jaw)
- Fine hair on the body (it’s called lanugo)
How Do You “Get” an Eating Disorder?
Ugh, if only there were more clear data. There’s no one thing experts can point to as a “cause” because it’s just not straight-forward, says Dr. Safer. Likely, it’s a combination of a bunch of things.
The way NEDA looks at this is by putting risk factors into categories: biological, psychological, and social. To be clear, even ticking off multiple items from these lists isn’t a clear-cut case for an eating disorder. But you are more at risk than someone without the same mix of factors.
Biological Risk Factors
- Genetics. “Eating disorders run in families, and the primary reason behind that is genetic,” says Dr. Bulik. According to studies, you have between a 3 and 12 percent higher chance of developing an eating disorder if a close relative has one.
- A history of dieting. While dieting doesn’t always morph into an eating disorder, people often diet for reasons that dovetail with EDs, such as being preoccupied with looking a certain way and using extreme measures to get there.
- Burning off more calories than you take in. Sometimes, in an effort to lose weight, excessive exercise pairs up with not eating enough. This combo can increase the chances of an eating disorder.
- Type 1 or type 2 diabetes. Diabulimia is a type of eating disorder specific to diabetes, where people try to control their weight through insulin resistance. Though researchers don’t know why having diabetes makes you more prone to an ED, adolescents with type 1 diabetes are 7 percent more likely to develop an eating disorder than those without diabetes.
Psychological Risk Factors
- Perfectionism. We live in a world that pats us on the head for straight As and awards curated Instagram photos with likes—so, for sure, being a perfectionist can exist outside of an ED. But it does tend to pre-empt the emergence of anorexia. “It’s something we really try to work on during treatment, to help people practice not being perfect and realizing that when they are not, the consequences are much less dire than they anticipated,” Dr. Bulik says.
- Body image dissatisfaction. When you’re really unhappy with your body, you’re more prone to engage in drastic behaviors so you can feel differently.
- History of an anxiety disorder: The genetic factors that spike your ED chances do the same for your anxiety risk. “Several studies have shown that anxiety disorders tend to come first in the majority, but not in all, patients,” Dr. Bulik says. “We have hypothesized that, especially in people with anorexia nervosa, starvation might actually make them feel less anxious. We don’t know what that mechanism is, but patients do report that.”
- Behavioral inflexibility. In laywomen’s terms, this translates to being a rigid rule-follower. Of course, just because you get to class on time or never wear white after Labor Day doesn’t mean you’re going to end up with an ED. The takeaway here is that people with an uncompromising mindset are more likely to apply those thought patterns toward food.
Social Risk Factors
- Weight stigma. It’s no newsflash that American culture applauds slenderness, or that there’s a stigma surrounding bigger bodies. Because of the deep lack of understanding around EDs, healthcare providers are more likely to diagnose underweight people, while people in larger bodies go under-diagnosed.
- Being teased or bullied. It sucks so bad that being bullied as a kid can put you at higher risk for another upsetting thing, but sadly research links the two. One theory: Bullying can contribute to having a poor body image, and an ED can be an attempt at gaining control.
- Feeling lonely. Nobody knows exactly why loneliness contributes to an ED, but scientists have observed a connection.
- Childhood trauma. Adults with EDs often report having been abused physically, mentally, or sexually as children. One recent study found people may use eating disorders as a way to dissociate from the trauma or, as the authors wrote, “escape from the conscious awareness of unbearable emotions and cognitive states.”
“The risk of developing any eating disorder is complex,” Dr. Bulik says. “It is not just risk genes that are passed down through the generations. One also has to consider protective genes, ones that might mitigate the effect of risk genes; environmental risk factors, such as teasing, bullying, or being in sports, arts, or professions that emphasize thinness; and environmental protective factors.”
Am I More Prone to Other Mental Health Issues?
Even though mental health conditions can be isolating, they rarely hang out alone. Like we said above re: EDs and anxiety disorders, the same biomarkers can put you at risk for both.
But it’s not just anxiety. Studies have also shown a correlation between eating disorders and depression, obsessive-compulsive disorder, and substance use disorder. Again, the big question still remains why.
With depression, while there are certainly multiple reasons, even researchers acknowledge how friggin’ distressing, frustrating, infuriating, all the “ings” it can be trying to fit society’s physical “ideal.” That can lead to dieting…which can lead to extreme dieting…which often leads to a diet fail…which can lead to shame and more depression because you feel like a failure. (BTW, it’s not you; the majority of people who diet gain back the weight.)
As for OCD, researchers have ID’d the relationship but not so much the explanation behind it. The best they’ve got is that it may, in part, relate to an innate need to control certain things. With substance abuse and EDs, the link could be due to personality traits.
The Treatment Options
Having an eating disorder can be all-encompassing. It’s real hard to go it alone—and so important to seek out help. Here’s a quick overview of some of the treatments available.
- Psychotherapy. You want—no, need—a therapist who is specially trained in eating disorders; look for one via Eating Disorder Hope’s database (also a great place to find nutritionists and other specialists in your area). “There are different types of psychotherapy, but the common goal is reducing eating disorder behaviors and identifying alternative coping mechanisms,” Altunkara says. “In certain types of psychotherapy, the therapist may focus on the patient’s beliefs, values, and cognitive processes to help them break the cycle that triggers disordered eating.”
- Support groups. Don’t let your ED be your only friend. There’s power in connecting with others who are working through something similar, whether IRL or virtual. Find a group through this database from Eating Disorder Hope.
- Nutritional counseling. As with psychotherapy, nutritional counseling will be based around your individual needs. But generally, says Dr. Bulik, the aim is to set regular eating times (our bodies crave predictability) and map out a plan for eating a healthy range and amounts of food (not too little and not too much).
- Medication. There is no magic pill for curing EDs—there aren’t even specific meds to treat it. But docs may give you an Rx to help with related concerns, such as depression and anxiety, Dr. Bulik says.
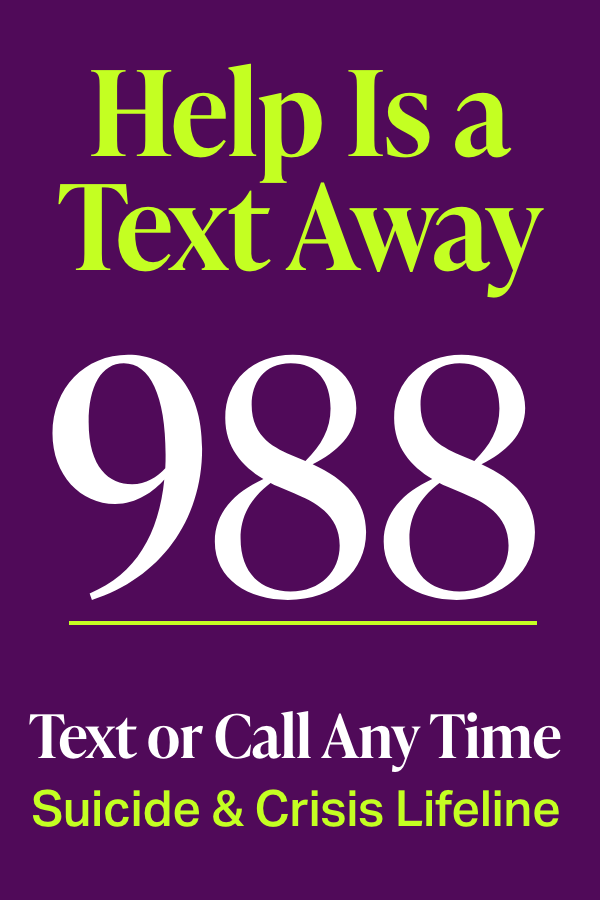
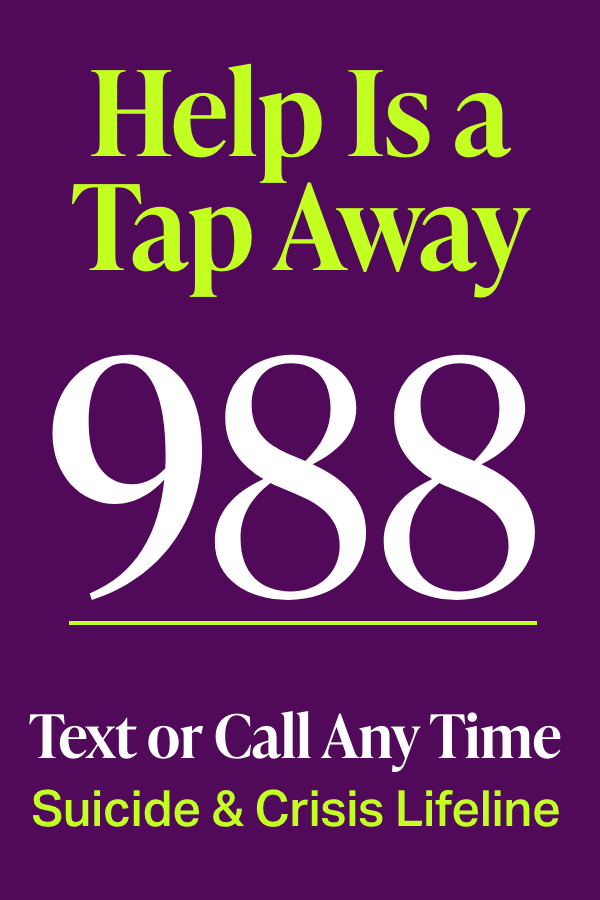
- Crisis helplines. Whether you need immediate help or have general questions, you can call or text ANAD at 888-375-7767.
Can I Recover From an Eating Disorder?
Lots of POVs on this, not a lot of stats. But we do know that, with help, you can curb disordered eating and live a full, amazing life. (Read that again!)
Dr. Small, for one, believes in recovery. “You have to work at it,” she says. “Recovery looks different to different people, and it looks different at different points in their recovery.” In other words, it isn’t always linear. There may be pitfalls and there may be setbacks, but it is possible to leave eating disorder behaviors in the past.
“Generally, treatment is more effective before an eating disorder becomes chronic, but even people with long-standing eating disorders can and do recover,” Dr. Small says. If you’re struggling, consider this your sign to seek help now and not wait.
Social Media Follows For a Healthier Mindset
Sure, there’s a lot of triggering stuff on social media. But there’s good out there, too.
1. NEDA
The National Eating Disorder Association is one of the most trusted sources in this space. They regularly bust myths and promote self-care on Instagram.
2. Jennifer Rollin, MSW
As an eating disorder therapist and someone who had an eating disorder herself, she knows what it’s like. Her IG is full of powerful mic drops that can help you form a more positive attitude toward eating and body image. She’s on TikTok, too!
3. Recovery Warriors
Yes, you can joke about recovery. This Instagram account posts relatable memes that’ll encourage and make you laugh.
4. Christy Harrison, R.D., C.D.N.
If part of what led to your eating disorder was dieting, this anti-diet dietitian can help prevent you from falling back into the trap. She’s not afraid to call out how the wellness and diet industries sneak up on us.
5. UNC Eating Disorders
The University of North Carolina Center of Excellence for Eating Disorders uses social media to share legit info about eating disorders. Knowledge is power
Weight Stigma and Social Media: https://www.frontiersin.org/articles/10.3389/fnut.2021.739056/full
Twitter Algorithm: https://www.theguardian.com/technology/2021/aug/10/twitters-image-cropping-algorithm-prefers-younger-slimmer-faces-with-lighter-skin-analysis
General Eating Disorder Statistics: https://anad.org/eating-disorders-statistics/
Eating Disorder Statistics Over Time: https://www.statista.com/statistics/979940/percentage-of-people-with-eating-disorders-us/
Statistics About Eating Disorder Deaths: https://www.hmpgloballearningnetwork.com/site/addiction/article/eating-disorders-rise-study-finds
Risk Factors For An Eating Disorder: https://www.nationaleatingdisorders.org/risk-factors
Anorexia Nervosa: https://www.ncbi.nlm.nih.gov/books/NBK459148/
Anorexia Nervosa Is Bad for Heart Health for People of Any Size: https://www.ucsf.edu/news/2019/11/415871/anorexia-nervosa-comes-all-sizes-including-plus-size
Bulimia Nervosa: https://www.ncbi.nlm.nih.gov/books/NBK562178/
Binge-Eating Disorder: https://www.ncbi.nlm.nih.gov/books/NBK551700/
Other Specified Feeding or Eating Disorder: https://www.nationaleatingdisorders.org/learn/by-eating-disorder/osfed
Heritability of Eating Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3599773/
Eating Disorders and Diabetes: https://pubmed.ncbi.nlm.nih.gov/32537669/
Body Dissatisfaction and Eating Disorders: https://pubmed.ncbi.nlm.nih.gov/12445588/
Anxiety and Anorexia Nervosa: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5782391/
Obesity and Eating Disorders: https://www.eatingdisorderhope.com/information/obesity-eating-disorders
Body Image and Eating Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6304369/
Bullying and Eating Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4715551/
Loneliness and Eating Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5670737/
Eating Disorders and Depression: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049372/
Eating Disorders and Obsessive-Compulsive Disorder:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993325/
Eating Disorders and Substance Abuse:
https://academic.oup.com/qjmed/article/99/5/335/2261057
Eating Disorders and Childhood Trauma: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7915652/